Abstract
Background
Hematopoietic cell transplantation (HCT) is a potentially curative therapy for patients with poor-risk MDS/AML, however, only a fraction of these patients are transplanted. Patients with TP53 mutated (TP53MUT) MDS/AML experience inferior clinical outcomes relative to TP53 wild type (TP53WT) patients which may be driven, in part, by lower HCT rates. We hypothesized that TP53MUT MDS/AML patients have unique risk factors that drive these reduced HCT rates.
Methods
Newly diagnosed, adult MDS/AML patients diagnosed between July 2015 and May 2019 with available NGS were retrospectively analyzed. TP53MUT was defined by loss of chromosome 17/17p by FISH and/or cytogenetics, or the presence of a TP53 mutation on NGS with VAF ≥1% at diagnosis. HLA typing was used as a surrogate for physician "intent to transplant." Disease risk was assessed using IPSS-R for MDS and ELN guidelines in AML for TP53WT patients. High or very high-risk MDS by IPSS-R, or adverse risk AML by ELN, were considered high-risk.
Results
Of 352 total patients, 39.8% had a primary diagnosis of MDS and 25.9% had TP53MUT disease. Median follow up was 1.2 years and 28% of patients underwent HCT at a median of 185 days after diagnosis. Presence of a TP53MUT was strongly associated with complex karyotype (CK) (87 vs 10%, p<0.001), monosomal karyotype (MK) (87 vs 10%, p<0.001), higher number of cytogenetic abnormalities (9.2 vs 1.0, p<0.001), and t-MDS/t-AML (29% vs 12%, p<0.001). TP53MUT patients had lower peripheral blood (PB) counts at diagnosis compared to TP53WT patients with PB blasts (12.9 vs 23.5%, p=0.029), WBC (mean: 12.6 vs 40.8 x103/mcL, p<0.001), hemoglobin (8.6 vs 9.4 gm/dL, p=0.002), and platelet count (78 vs 108 x103/mcL, p=0.002).
Intent to transplant was similar between the TP53MUT and TP53WT groups (50 vs 52%). In multivariate analyses, TP53MUT patients had 3.1x greater odds (95% CI: 1.4 - 6.7) of HLA typing, however, HCT rates were significantly lower compared to all-risk TP53WT patients (19 vs 31%, p=0.028). In a subgroup analysis of high-risk MDS/AML patients (n=167), intent to transplant was similar between TP53MUT and TP53WT groups (52% vs 60%), however, HCT rates were lower compared to other high-risk TP53WT patients (19 vs 31%, p=0.082).
TP53MUT MDS/AML patients with intent to transplant received more lines of therapy (mean: 2.1 vs 1.0, p<0.001), experienced fewer infection-related treatment interruptions (11% vs 34%, p=0.013), and had higher CR rates (44% vs 4.5%, p=<0.001). These patients experienced a greater number of days with neutropenia (79 days vs 62 days, p=0.023) and trend toward more infectious complications (mean: 1.7 vs 1.4, p=0.071).
In multivariate analysis of intent to transplant patients, TP53MUT was not associated with increased odds of transplant (OR 0.64, 95% CI: 0.29-1.42). Time to transplant was similar between TP53MUT and TP53WT patients (median: 169 vs 186 days, p=0.18).
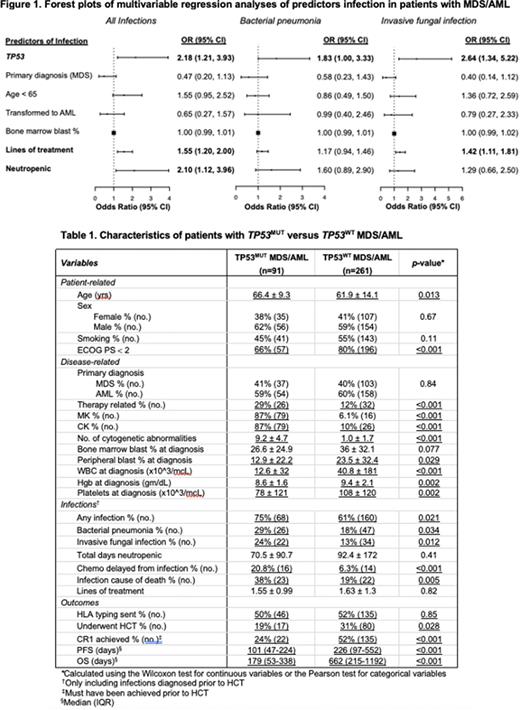
TP53MUT MDS/AML patients had a significantly higher number of infections than their TP53WT counterparts. A greater percentage of TP53MUT patients had ≥1 infection during their course (75% vs 61%, p=0.021) and the number of unique infections per patient was significantly higher than TP53WT patients (1.5 vs 1.2, p=0.002). Bacterial pneumonias (29% vs 18%, p=0.034), invasive fungal (24% vs 13%, p=0.012), gastrointestinal (19% vs 10%, p=0.04), and urinary infections (15.4% vs 8%, p=0.044) were more prevalent in TP53MUT patients. TP53MUT patients were more likely to die of an infection (38% vs 19%, p=0.005) despite similar duration of neutropenia (71 vs 92 days, p=0.41). In multivariate analyses, TP53MUT was independently associated with increased odds of infection (OR 2.18, 95% CI: 1.21-3.93), including bacterial pneumonia (OR 1.83, 95% CI: 1.00-3.33), and invasive fungal infection (OR 2.64, 95% CI: 1.34-5.22). Infectious complications were associated with increased hazard of death (HR 1.46, 95% CI: 1.09-1.96) and reduced odds of HCT (OR 0.42, 95% CI 0.19-0.90) (Figure 1).
Conclusions
Patients with TP53MUT MDS/AML have lower HCT rates compared other, poor-risk TP53WT MDS/AML patients despite a comparable intent to transplant. Our work demonstrates that TP53MUT is an independent risk factor for infection which likely contributes to the lower HCT rates and poor survival reported in this population. Measures to reduce infectious complications may improve HCT rates and outcomes in patients with TP53MUT MDS/AML.
Disclosures
Kishtagari:CTI Biopharm: Speakers Bureau. Dholaria:Angiocrine: Research Funding; MJH Biosciences: Honoraria; Arivan: Consultancy; BMS: Research Funding; Jazz Pharmaceuticals: Consultancy; MEI Pharma: Research Funding; Takeda: Research Funding; Wugen: Research Funding; Vanderbilt University Medical Center: Current Employment; Janssen: Research Funding; Gamida Cell: Consultancy; Orca Bio: Research Funding; Molecular Templates: Research Funding; Poseida: Research Funding; Pfizer: Research Funding; BEAM Therapeutics: Consultancy. Kim:Agenus: Consultancy; Nextcure: Research Funding. Savona:Bristol Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: travel expenses; Takeda: Consultancy; Taiho Pharmaceutical: Consultancy; Karyopharm Therapeutics: Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees; ALX Oncology: Research Funding; Astex Pharmaceuticals: Research Funding; Sierra Oncology: Consultancy, Other: travel expenses; Geron: Consultancy; TG Therapeutics: Consultancy, Other: Travel expenses, Research Funding; Incyte Corporation: Research Funding; Forma: Consultancy; Ryvu Therapeutics: Consultancy, Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy; AbbVie: Consultancy, Other: travel expenses. Byrne:Celularity, Concert: Consultancy, Other: DSMC; Karyopharm: Research Funding; Taiho: Research Funding; CTI: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal